
A 57-year-old male presents to the clinic with complaints of abdominal pain in the epigastric region radiating to the back. Pain worsens postprandially, usually after a heavy meal. Episodes have occurred on and off the last six months, with pain being dull but moderate to intense at times, consistent with his known diagnosis of chronic pancreatitis. He is a smoker of one pack per day, with a 30-year history, and has not committed to quitting. His main complaint today is the recent development of steatorrhea and a 10-pound unintentional weight loss in the last four weeks. He has not refilled his pancreatic enzymes in the past month.
What lifestyle factors should be recommended to this patient to minimize his symptoms overall?
A) Compliance with pancreatic enzyme replacement therapy
B) Eat four to five small meals per day
C) Smoking cessation
D) Eat a high-protein, low-fat diet
E) All of the above
The correct answer is E, all of the above. Many lifestyle factors play a role in the management of chronic pancreatitis.
Practice Pearls
General
- Chronic pancreatitis is defined as a progressive inflammatory disorder that leads to irreversible destruction of exocrine and endocrine pancreatic parenchyma caused by atrophy and/or replacement with fibrotic tissue.1
- Environmental and genetic factors can play a role in the disease process, with cigarette smoking and alcohol use being the most common.
- Up to 80 percent of patients with chronic pancreatitis will develop abdominal pain. Steatorrhea is the second most common symptom. A subset of patients with chronic pancreatitis are asymptomatic.2
- Complications of chronic pancreatitis include exocrine pancreatic insufficiency, diabetes (endocrine pancreatic insufficiency), metabolic bone disease, pancreatic cancer and anatomic complications (pancreatic duct stricture, pancreatic and/or bile duct obstruction, duodenal obstruction, pseudocyst formation, splenic vein thrombosis).2
- The causes of chronic pancreatitis can be remembered using the acronym TIGAR-O.3
T = toxic-metabolic (alcohol, smoking, hypertriglyceridemia)
I = idiopathic
G = genetic (hereditary pancreatitis, pathogenic variants of PRSS1, SPINK1, CFTR, CTRC)
A = autoimmune pancreatitis
R = recurrent acute pancreatitis
O = obstruction (chronic) of the main pancreatic duct
Diagnosis
- A comprehensive review of all risk factors should be conducted in all patients with clinical features of chronic pancreatitis.4
- A CT or MRI is the first-line test of choice in diagnosing chronic pancreatitis.2
- A secretin-stimulated MRCP can define subtle changes in the pancreatic ducts.1
- Endoscopic ultrasound is the best imaging modality to assess for parenchymal and ductal changes in early chronic pancreatitis.1
- ERCP, previously the traditional route for diagnosis, has been replaced with MRCP and EUS. ERCP should only be used if a therapeutic intervention is needed.
- Laboratory assessment includes CBC, BMP, LFTs, lipase, amylase, lipid panel and fecal elastase value. Lipase and amylase can be elevated but are often normal, secondary to significant scarring and fibrosis of the pancreas (even during an episode of pain).
- If autoimmune pancreatitis is suspected, labs should include ESR, CRP, ANA, RF, antibodies and immunoglobulins (total IgG and IgG4).
- A 72-hour quantitative fecal fat test is the gold standard for diagnosing exocrine pancreatic insufficiency but is very difficult for patients to accurately complete. Alternatively, pancreatic fecal elastase is often performed. This test can be completed on a single, formed stool sample; it is not altered by using pancreatic enzymes.
Figure 1: Chronic pancreatitis on MRCP
Shown below: dilated main duct and large side branches shown on MRCP.
Image courtesy of Mohammad Ali Al-Haddad, MD, Indiana University School of Medicine
Figure 2: Chronic pancreatitis on MRCP
From left to right: a stricture in the pancreatic head, dilated side branches in the head, dilation of the duct upstream to the stricture and multiple dilated branches in the body and tail.
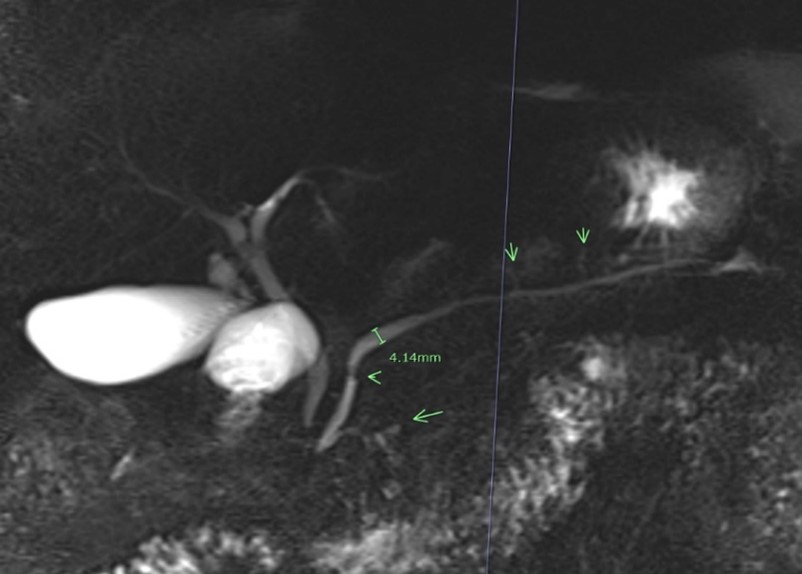
Image courtesy of Temel Tirkes, MD, Indiana University Radiology
Treatment
- The main goal is to decrease pain and improve malabsorption.
- Educating the patient on small frequent meals and replacing fat-soluble vitamins and pancreatic enzyme replacement therapy is recommended, as is counseling by a registered dietician.
- Cessation of smoking and alcohol is imperative to prevent disease progression.4
- Nonopioid pain management options include the use of tricyclic antidepressants and nonsteroidal anti-inflammatory drugs.
- Antioxidant therapy is an area of research that may be helpful, but optimal regimens and doses have not been defined.2
- Endoscopic ultrasound-guided or percutaneous celiac plexus block can be used for pain management. This is temporary and, if effective, will likely require repeated blocks over time.4
- For patients with obstructive disease, endoscopic management is recommended first-line with ERCP and pancreatic duct endotherapy (balloon dilatation, pancreatic duct stenting).
- EUS-guided pseudocyst drainage can also be performed for symptomatic pseudocysts (asymptomatic pseudocysts do not require intervention).
- Surgical consultation should be performed if patients fail endoscopic management.4

Sarah Stainko, MSN, NP-C
Indiana University Health Physicians
Indianapolis, IN
Sarah Stainko, MSN, NP-C, is a board-certified nurse practitioner in the Division of Gastroenterology and Hepatology at Indiana University Health in Indianapolis, Indiana. She works in the area of Destination Services, Innovative Endoscopy and Motility.
- Benjamin O, Lappin SL. Chronic Pancreatitis. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. https://www.ncbi.nlm.nih.gov/books/NBK482325/
- Hart PA, Conwell DL. Chronic pancreatitis: managing a difficult disease. Am J Gastroenterol. 2020;115:49-55. doi: 10.14309/ajg.0000000000000421
- Forsmark CE, Freedman SD, Lewis MD. Etiology and pathogenesis of chronic pancreatitis in adults. UptoDate. Updated March 11, 2024. https://www.uptodate.com/contents/etiology-and-pathogenesis-of-chronic-pancreatitis-in-adults?search=chronic%20pancreatitis&source=search_result&selectedTitle=4%7E150&usage_type=default&display_rank=4#H1922599546
- Gardner TB, Adler DG, Forsmark CE, Sauer BG, Taylor JR, Whitcomb DC. ACG Clinical Guideline: Chronic Pancreatitis. Am J Gastroenterol. 2020;115:322-339. doi: 10.14309/ajg.0000000000000535