
A 30 year-old male with a history of cystic fibrosis and PEG tube dependency presents to clinic with complaints of difficulty using PEG tube, leaking around tube and abdominal pain. He first started noticing these problems 4 days ago. Prior to this he has been doing well with his feeds and has been able to gain 15 lb. PEG tube was placed 8 months prior to presentation. On exam, he is well appearing and in no acute distress. He is afebrile. PEG tube is located within LUQ. The external bumper is tight on his skin. There is leakage of what appears to be gastric contents around his tube with some mild skin break down beneath bumper and erythema. No frank pus is appreciated. No warmth or streaking. You attempt to twist tube, but are unable to do so, and the maneuver causes severe pain. When you attempt to flush the tube with water, there is significant resistance.
What is the most likely diagnosis?
- PEG site cellulitis
- Buried bumper syndrome
- Tube clogging due to formula residue
- Accidental PEG dislodgement into peritoneal cavity
Show Answer
The correct answer is B, Buried bumper syndrome.
Practice Pearls
Pathogenesis/Pathology
- Buried bumper syndrome occurs when the internal bumper migrates and becomes embedded within gastric wall or gastrostomy tract with partial or complete growth of gastric mucosa over internal bumper
- Occurs in ~1% (0.3-2.4%) of patients w gastrostomy tubes
- Typically occurs months to years after tube placement, although may present within weeks of placement
- Risk factors:
- Excessive tension between internal and external bumper
- Malnutrition
- Poor wound healing
- Significant weight gain secondary to enteral nutrition
- Buried bumper syndrome may be complicated by GI bleeding, perforation, intra-abdominal and abdominal abscesses, and these complications can lead to fatal outcomes
Clinical Manifestations
- Pain at tube site
- Inability to move or rotate tube
- Difficulty running feeds/flushing
- Leakage around tube
- Infection
Diagnosis
- May be diagnosed based on clinical presentation
- Confirmed via endoscopy
- Endoscopic view of buried bumper
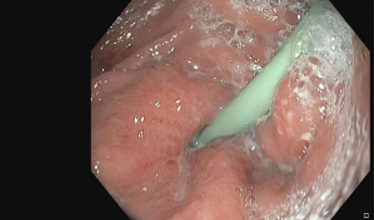
Image from personal library of Katelyn Cookson
Figure 1. Gastric Body, buried internal bumper
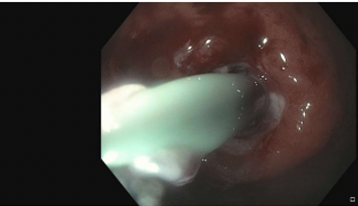
Images from personal library of Katelyn Cookson
Figure 2. Gastric Body, pus draining from gastric defect
- Radiologic work up
- US:
- Rapid, noninvasive
- Highly sensitive and specific for buried bumper syndrome
- Findings will identify internal bumper embedded within gastric wall, often with hyperechoic tissue overgrowth
- CT:
- Will identify internal bumper located outside of gastric lumen, may have surrounding soft tissue thickening, inflammatory changes, or abscess formation
- Provides detailed anatomical localization
- Allows for assessment of possible complications (abscess formation, perforation…)
- Contrast study should be performed prone as contrast may falsely appear to safely pass through the imbedded bumper into gastric lumen
- Axial CT image of buried bumper

Image source : https://doi.org/10.53347/rID-148034
Figure 3. Axial CT Image, baby bumper
Management
- EGD is indicated in all cases where BBS is suspected
- If internal bumper remains within lamina muscularis propria, may be removed endoscopically
- Replacement PEG may be placed at same time as removal
- If internal bumper is localized outside of stomach, patient will require treatment with surgical team
- Antibiotics are not necessary in all cases of BBS, but are indicated if there is concern for infection or associated abscess
- Prevention centers on maintaining adequate spacing between skin and external bumper (~1 cm)
References
- Itkin M, DeLegge MH, Fang JC, et al. Multidisciplinary Practical Guidelines for Gastrointestinal Access for Enteral Nutrition and Decompression from the Society of Interventional Radiology and American Gastroenterological Association (AGA) Institute, with Endorsement by Canadian Interventional Radiological Association (CIRA) and Interventional Radiological Society of Europe (CIRSE) doi:10.1016/j.jvir.2011.04.006.
- Cyrany J, Rejchrt S, Kopacova M, Bures J. Buried bumper syndrome: A complication of percutaneous endoscopic gastrostomy. World J Gastroenterol. 2016;22(2):618-627. doi:10.3748/wjg.v22.i2.618
- Micic D, Martin JA, Fang J. AGA Clinical Practice Update on Endoscopic Enteral Access: Commentary doi:10.1053/j.gastro.2024.09.043.
Author

Katelyn Cookson, PA-C is a Physician Assistant specializing in Gastroenterology at UCHealth Digestive Health Center and is also an Instructor at University of Colorado Anschutz Medical Campus. Katelyn serves as co-Chair the ASGE APP Committee.